Discover how AI nutrition coaching apps are disrupting traditional healthcare approaches, challenging medical orthodoxy with personalized, data-driven wellness solutions that work 24/7.
The stethoscope around your neck might soon feel as outdated as a flip phone. While healthcare professionals debate the ethics of AI diagnosis, a quiet revolution is unfolding in patients’ pockets—one that’s rewriting the rules of nutritional guidance without waiting for medical committees to catch up.
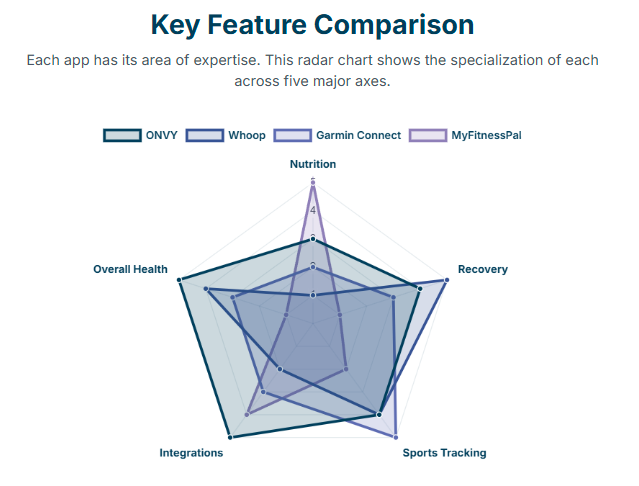
Four platforms are leading this insurgency: ONVY’s holistic performance optimization, Whoop’s recovery-focused ecosystem, Garmin Connect’s athletic prowess, and MyFitnessPal’s nutritional democracy. But this isn’t just another app comparison. This is about understanding how artificial intelligence is fundamentally challenging the traditional doctor-patient relationship in nutrition, and why healthcare professionals who ignore this shift do so at their own peril.
The Unspoken Truth About Traditional Nutritional Counseling
Let’s address the elephant in the consultation room. Traditional nutritional counseling operates on a model that would make any tech entrepreneur cringe: infrequent touchpoints, generic recommendations, and zero real-time feedback. A patient receives dietary advice during a 15-minute consultation, then disappears into the wild for three months with nothing but a printed sheet and good intentions.
This approach worked when our understanding of metabolism was limited to calories in, calories out. But we now know that nutrition is a complex, dynamic system influenced by sleep quality, stress levels, physical activity, circadian rhythms, and even heart rate variability. The human body doesn’t operate on office hours, so why should nutritional guidance?
Enter AI Nutrition Coaching platforms that monitor, analyze, and advise around the clock. These aren’t just calorie counters with fancy interfaces—they represent a philosophical shift from episodic care to continuous health optimization.
The Four Horsemen of Nutritional Disruption
ONVY: The Performance Whisperer
ONVY doesn’t play the traditional nutrition game. Instead of asking users to log meals obsessively, it takes a radical approach: analyzing recovery data, heart rate variability, and stress markers to provide indirect nutritional guidance. This platform understands something that many healthcare professionals miss—nutrition isn’t just about what you eat; it’s about how your body processes and recovers from everything you put it through.
The genius lies in its device agnosticism. While healthcare systems struggle with interoperability, ONVY seamlessly integrates data from Apple Watch, Oura Ring, Whoop, and Garmin devices. It’s creating the unified health dashboard that electronic medical records promised but never delivered.
Whoop: The Recovery Prophet
Whoop made a counterintuitive bet that proved brilliant: focus entirely on recovery metrics and let users connect their own nutritional dots. By providing precise data on how sleep quality, heart rate variability, and strain scores fluctuate, Whoop enables users to become their own nutritional detectives.
This indirect approach often proves more effective than direct coaching. When users see their recovery scores plummet after a night of poor eating, the lesson sticks better than any dietary lecture. Whoop understood behavioral psychology before it became a buzzword in digital health.
Garmin Connect: The Athletic Purist
Garmin Connect represents the intersection of serious athletic performance and nutritional optimization. While it doesn’t offer native nutritional coaching, its integration capabilities and comprehensive activity tracking create a foundation that many sports nutritionists find more valuable than traditional food logging apps.
The platform’s strength lies in its understanding that athletes don’t need another calorie counter—they need precise energy expenditure calculations, hydration tracking, and performance correlations that help optimize fueling strategies for specific activities.
MyFitnessPal: The Democratized Nutritionist
With over 200 million users, MyFitnessPal achieved something remarkable: it made nutritional awareness accessible to the masses. While its AI capabilities remain relatively simple, its vast food database and barcode scanning functionality democratized nutritional tracking in ways that healthcare systems couldn’t match.
The platform’s real innovation wasn’t technological—it was sociological. By gamifying nutrition tracking and building community features, MyFitnessPal proved that patients would engage with nutritional guidance if you made it convenient and social.
The Clinical Implications Nobody’s Discussing
These platforms are generating unprecedented amounts of longitudinal nutritional and biometric data. We’re talking about millions of users providing real-time feedback on how different foods, timing strategies, and dietary patterns affect their recovery, performance, and wellbeing.
This data goldmine raises uncomfortable questions for healthcare professionals. When an AI platform analyzing thousands of similar users suggests that intermittent fasting might benefit a specific patient based on their sleep patterns and activity levels, how does that compare to generalized dietary guidelines from a 20-minute consultation?
The answer isn’t that AI platforms will replace nutritionists or physicians. The answer is that they’re creating informed patients who arrive at appointments with sophisticated questions and expectations that traditional healthcare delivery models aren’t equipped to handle.
The Personalization Paradox
Traditional medical training emphasizes evidence-based medicine, but what happens when AI platforms can provide n=1 evidence for each individual patient? These platforms track how specific foods affect sleep quality, recovery metrics, and performance indicators for each user individually.
ONVY might notice that a user’s heart rate variability drops consistently after consuming dairy products. Whoop could identify that late-evening carbohydrate intake correlates with poor sleep quality for a specific individual. Garmin might detect that pre-workout nutrition timing significantly impacts training performance.
This level of personalization challenges the one-size-fits-all dietary recommendations that form the backbone of traditional nutritional counseling. We’re moving from population-based guidelines to individual optimization algorithms.
The Integration Challenge Healthcare Can’t Ignore
The most sophisticated healthcare systems still struggle with basic data sharing between departments. Meanwhile, these consumer platforms seamlessly integrate sleep data from one device, activity metrics from another, and nutritional information from a third source to provide holistic insights.
Healthcare professionals who dismiss these platforms as “just consumer gadgets” are missing a critical point: patients are already using these tools to make health decisions. The question isn’t whether these platforms are perfect—it’s whether healthcare professionals are prepared to engage with patients who arrive armed with months of biometric data and AI-generated insights.
The Future of Nutritional Guidance Is Already Here
The convergence of continuous glucose monitors, wearable devices, and AI platforms is creating a new category of nutritional guidance that operates in real-time. Imagine receiving a notification that your current stress levels and sleep debt suggest avoiding caffeine for the next four hours, or that your recovery metrics indicate you should increase protein intake by 15% for the next three days.
This isn’t science fiction—it’s the logical evolution of the data these platforms are already collecting. The technology exists; we’re simply waiting for the algorithms to become more sophisticated and the integrations to become more seamless.
What Healthcare Professionals Must Understand
The patients walking into your clinics are increasingly data-literate and expect personalized recommendations based on their individual metrics. They’ve been tracking their heart rate variability, sleep efficiency, and dietary patterns for months or years. They want to understand why their AI coach’s recommendations might differ from your clinical guidelines.
This isn’t about replacing professional medical advice—it’s about elevating the conversation. When patients arrive with sophisticated self-knowledge and specific questions about their biometric data, healthcare professionals have an opportunity to provide context, interpretation, and clinical oversight that AI platforms cannot match.
The Ethical Minefield We’re Walking Into
These platforms raise profound questions about data privacy, algorithmic bias, and the medicalization of daily life. When AI systems make nutritional recommendations based on biometric data, who bears responsibility for the outcomes? How do we ensure that AI coaching doesn’t perpetuate existing health disparities or create new forms of digital divide?
The democratization of nutritional guidance through AI platforms could reduce healthcare disparities by making sophisticated coaching available to anyone with a smartphone. Alternatively, it could exacerbate inequalities if premium features remain behind paywalls or if algorithmic recommendations reflect biases present in training data.
The Call for Healthcare Innovation
Healthcare professionals have a choice: embrace this technological shift as an opportunity to enhance patient care, or resist it until disruption becomes inevitable. The patients using these platforms aren’t looking to replace their healthcare providers—they’re looking for providers who can help them make sense of the data they’re collecting and the insights they’re receiving.
The future belongs to healthcare professionals who can bridge the gap between AI-generated insights and clinical expertise. Those who learn to interpret wearable data, understand the capabilities and limitations of AI coaching platforms, and integrate this information into comprehensive care plans will provide irreplaceable value to their patients.
The revolution isn’t coming—it’s already here, running quietly on millions of smartphones, collecting data while patients sleep, and generating insights that challenge traditional approaches to nutritional guidance. The question isn’t whether AI will transform nutritional counseling; it’s whether healthcare professionals will lead that transformation or be left scrambling to catch up.
The stethoscope isn’t obsolete yet, but it’s sharing space with algorithms that never sleep and insights that update in real-time. Welcome to the future of nutritional medicine—where artificial intelligence meets human wisdom, and both are necessary for optimal patient care.
Recommended Reading:
- The Digital Doctor by Dr. Robert Wachter – navigating technology in healthcare
Sources:
- American Journal of Preventive Medicine: Digital Health Interventions in Nutrition
- Nature Digital Medicine: Wearable Technology and Health Outcomes
- JAMA Internal Medicine: AI Applications in Clinical Practice
Disclaimer: This educational content was developed with AI assistance by a physician. It is intended for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare professional for personalized guidance. The information provided is valid as of the date indicated at the end of the article.

Comments