Intermittent Fasting AI
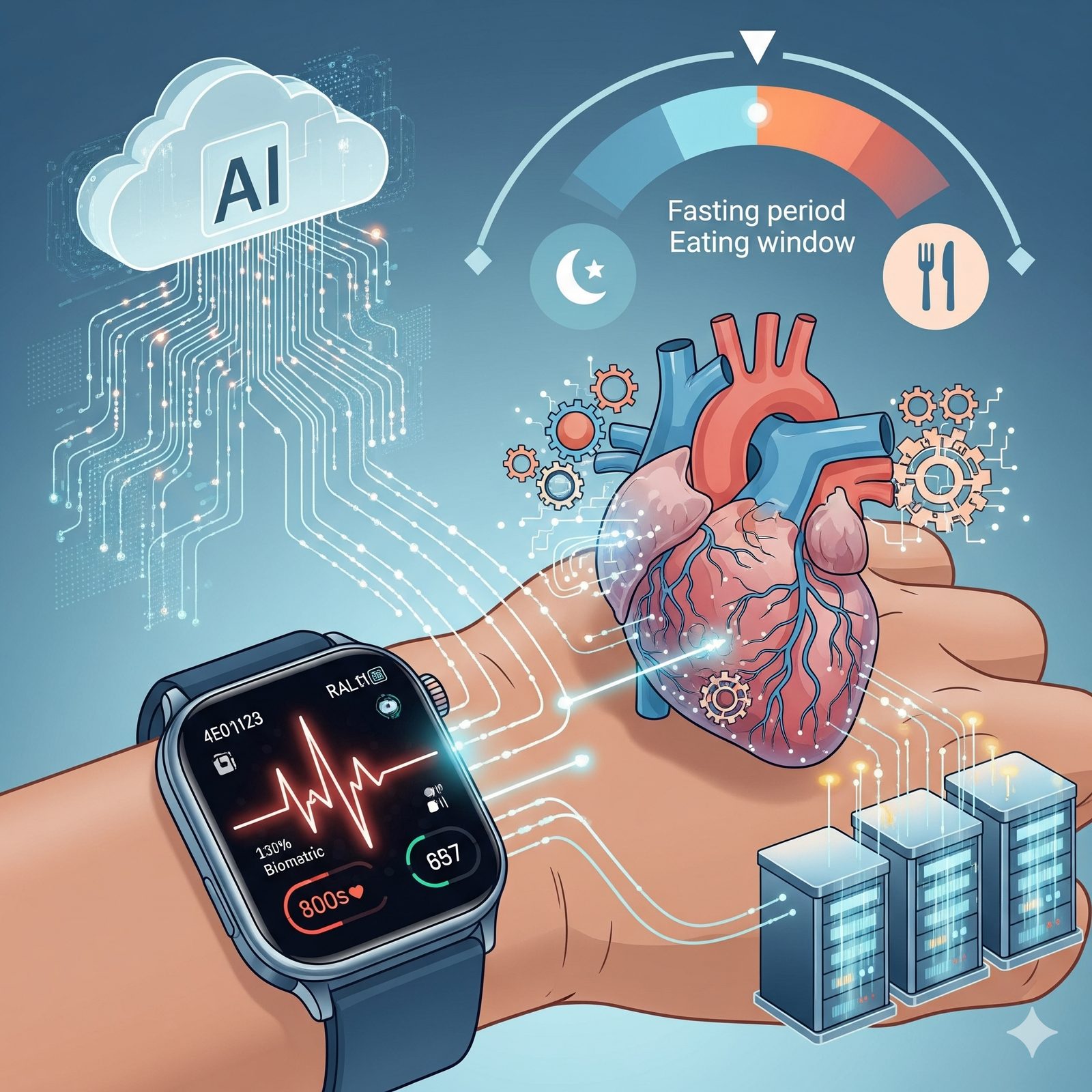
Intermittent fasting AI monitoring could revolutionize personalized medicine, but new cardiovascular risks challenge everything we thought we knew about time-restricted eating.
Picture this: your smartwatch buzzes at 2 PM with a gentle warning—”Your Intermittent Fasting AI health coach suggests ending your eating window now to optimize cardiovascular outcomes.” Science fiction? Not anymore. We’re living in an era where artificial intelligence can predict your metabolic state with 90% accuracy, yet a bombshell study from the American Heart Association suggests that intermittent fasting—the darling of biohackers worldwide—might be quietly killing people.
Welcome to the messy, contradictory, and absolutely fascinating intersection of ancestral eating patterns and cutting-edge AI. As a medical biologist who’s spent years watching health trends crash against scientific reality, I’m here to decode this paradox that’s reshaping how we think about personalized nutrition.
The stakes couldn’t be higher. Intermittent fasting has exploded from a niche biohacking practice to a mainstream phenomenon affecting millions of lives. Meanwhile, AI-powered health monitoring is transitioning from experimental labs to everyday wearables. But when promising interventions meet concerning safety signals, we need more than hype—we need nuanced understanding.
The Intermittent Fasting Revolution: Promise Meets Peril
Let me be blunt: intermittent fasting works. The metabolic benefits are undeniable and impressive. When patients restrict their eating to specific windows—whether the popular 16:8 method or more aggressive protocols—their bodies undergo remarkable transformations. Insulin sensitivity improves dramatically, with HbA1c reductions of 3-6%. Weight loss averages 5-8% of body weight within 8-12 weeks. Inflammatory markers like CRP and IL-6 plummet. Triglycerides drop by 20-30%.
These aren’t marginal improvements—they’re clinically significant changes that can transform someone’s metabolic trajectory. The mechanisms make biological sense too. During fasting periods, glycogen stores deplete, forcing the body to mobilize fatty acids and enter ketogenesis. This metabolic flexibility, largely absent in our constantly-fed modern lifestyle, appears to be a powerful lever for health optimization.
But here’s where things get uncomfortable for the intermittent fasting community: the American Heart Association’s 2024 observational study involving over 20,000 adults followed for eight years revealed a 91% increased risk of cardiovascular death among those practicing 16:8 intermittent fasting compared to those maintaining 12-16 hour eating windows.
Now, before the IF evangelists dismiss this as flawed observational research (which it partially is), let’s acknowledge what this signal represents. When a study of this magnitude flags a nearly doubled mortality risk, we need to pause and think critically, not defensively.
Why Your Circadian Clock Might Be Your Heart’s Enemy
The cardiovascular risk mechanism isn’t mysterious—it’s rooted in evolutionary biology. Our cardiovascular system evolved with predictable eating patterns aligned to circadian rhythms. When we compress eating into narrow windows, especially when poorly timed, we create what I call “metabolic whiplash.”
Consider this: prolonged fasting triggers stress hormone cascades involving cortisol and adrenaline. While acute stress responses can be beneficial, chronic activation potentially damages endothelial function—the delicate inner lining of blood vessels. Add circadian desynchronization (eating late or skipping meals at biologically optimal times), and you’ve created a perfect storm for cardiovascular dysfunction.
The timing matters enormously. Research consistently shows that early feeding—finishing your last meal by 2-4 PM—produces superior glycemic control compared to late feeding patterns like skipping breakfast. This isn’t just about calories; it’s about honoring our biological programming.
Here’s what mainstream IF advocates won’t tell you: the same metabolic flexibility that makes intermittent fasting powerful also makes it potentially dangerous. When you’re metabolically healthy and young, your body handles these transitions gracefully. But layer in cardiovascular disease, diabetes, advanced age, or chronic stress, and those same mechanisms can become liability.
Enter AI: The Game-Changing Personalization Engine
This is where artificial intelligence transforms everything. Instead of applying one-size-fits-all intermittent fasting protocols, AI enables genuinely personalized approaches that could eliminate the risks while maximizing benefits.
Think of AI health monitoring as having a sophisticated medical team analyzing your physiology 24/7. Your smartwatch tracks heart rate variability, sleep patterns, activity levels, and stress indicators. Continuous glucose monitors provide real-time metabolic feedback. Advanced algorithms process this data against vast datasets from thousands of similar individuals to predict optimal fasting windows, identify early warning signs, and adjust protocols dynamically.
The precision is remarkable. AI can determine your fasting state with 90% accuracy by analyzing patterns invisible to human perception. Imagine algorithms that recognize when your heart rate variability suggests metabolic stress, when your glucose patterns indicate insulin resistance, or when your sleep data reveals circadian disruption from poorly timed eating.
A pilot study with post-heart attack patients demonstrated this potential beautifully. When 112 STEMI patients followed AI-guided 5:2 protocols, they showed 5.2% improvement in heart function compared to 1.8% in controls, alongside 34% reduction in inflammatory markers. While preliminary, these results suggest that proper personalization and monitoring could transform intermittent fasting from a population-level risk into an individualized therapeutic tool.
The Precision Medicine Promise: Beyond One-Size-Fits-All
Here’s my controversial opinion: most intermittent fasting advice is dangerously generic. Telling a 65-year-old diabetic to follow the same 16:8 protocol as a healthy 30-year-old athlete isn’t just ineffective—it’s potentially harmful.
AI changes this equation fundamentally. Instead of rigid eating windows, imagine adaptive protocols that respond to your real-time physiology. Stressed about a work deadline? Your AI might recommend extending your eating window. Recovering from illness? The algorithm adjusts fasting intensity accordingly. Glucose levels trending upward? The system modifies timing to optimize metabolic response.
This isn’t futuristic speculation—we’re seeing early implementations today. Machine learning algorithms can predict weight loss success rates, identify individuals prone to eating disorders, and flag early signs of metabolic complications before they become clinically apparent.
The key insight is that intermittent fasting effectiveness depends on dozens of variables: age, sex, metabolic health, chronotype, stress levels, sleep quality, exercise patterns, and genetic factors. Only AI has the computational power to integrate these complex interactions into actionable recommendations.
Risk Stratification: Who Should Fast, Who Should Run
Let’s get practical about risk assessment. Based on current evidence, here’s my clinical framework:
Green light candidates include metabolically healthy adults under 50 with stable circadian rhythms, good stress management, and no eating disorder history. These individuals can experiment with progressive protocols starting with 14:10 windows and monitoring biomarkers quarterly.
Yellow light cases require careful supervision: controlled type 2 diabetics, individuals with cardiovascular risk factors, and those over 50. These patients need medical oversight, glucose monitoring, and conservative approaches like 12:12 protocols with gradual progression.
Red light populations where I recommend avoiding intermittent fasting entirely include patients with cardiovascular disease history, eating disorders, advanced age with frailty, pregnancy or breastfeeding, and active mental health conditions. The risks simply outweigh potential benefits.
The warning signs to immediately discontinue fasting are crystal clear: persistent fatigue, frequent dizziness, heart palpitations, severe mood changes, food obsessions, or rapid weight loss exceeding 1kg weekly. These aren’t minor side effects—they’re danger signals requiring immediate intervention.
The Future of Personalized Nutrition: Beyond Hype
Here’s what excites me about the convergence of AI and nutrition science: we’re moving beyond population studies toward n-of-1 medicine. Instead of asking “Does intermittent fasting work?” we can ask “Does this specific protocol work for this individual at this time?”
The implications extend far beyond intermittent fasting. We’re witnessing the birth of truly personalized nutrition, where dietary recommendations adapt continuously to changing physiology, life circumstances, and health goals. Your smartphone could become the most sophisticated nutritional counselor ever created, learning your patterns, predicting responses, and optimizing interventions in real-time.
But let’s address the elephant in the room: algorithmic bias and over-medicalization. AI systems trained primarily on young, healthy, predominantly male populations might not generalize to diverse demographics. There’s also risk of creating anxiety around normal physiological variations or promoting obsessive health monitoring behaviors.
The solution isn’t avoiding AI—it’s demanding better AI. We need diverse training datasets, transparent algorithms, and integration with human clinical judgment rather than replacement of it.
Clinical Integration: Bridging Innovation and Practice
For healthcare providers reading this, the message is clear: AI-augmented intermittent fasting represents a paradigm shift requiring new competencies. We need protocols for interpreting AI recommendations, systems for integrating wearable data into electronic medical records, and frameworks for liability when algorithms make clinical suggestions.
The most successful implementations I’ve observed combine AI insights with human wisdom. Algorithms excel at pattern recognition and continuous monitoring, but clinicians provide context, empathy, and judgment calls that remain irreplaceably human.
Training requirements are substantial. Healthcare providers need fluency in interpreting algorithmic outputs, understanding limitations and biases, and communicating AI-generated recommendations to patients effectively. We also need robust validation studies proving that AI-guided protocols improve outcomes compared to standard care.
The Verdict: Cautious Optimism Over Blind Faith
After dissecting the evidence, here’s my synthesis: intermittent fasting is a powerful metabolic intervention that’s been applied too broadly and too rigidly. The cardiovascular risk signals are real and concerning, but they likely reflect poor implementation rather than inherent dangers.
AI offers a path forward—not through eliminating human judgment, but by augmenting our ability to personalize interventions precisely. We’re moving from crude population-based recommendations toward sophisticated, individualized protocols that adapt continuously to changing physiology.
The most important lesson? Medicine is becoming increasingly personalized, and one-size-fits-all approaches are becoming obsolete. Whether we’re discussing intermittent fasting, medication dosing, or exercise prescriptions, the future belongs to algorithms that treat you as an individual, not a statistical average.
For patients considering intermittent fasting: demand personalization, insist on monitoring, and remain skeptical of universal claims. For healthcare providers: embrace AI tools while maintaining clinical judgment and prioritizing patient safety over trendy interventions.
The convergence of ancient eating patterns and modern AI represents medicine at its most exciting—rigorous yet innovative, personalized yet scalable, promising yet appropriately cautious. We’re not just optimizing metabolism; we’re reimagining how humans interact with food, technology, and their own biology.
In this brave new world of AI-guided health optimization, the smartest approach isn’t blind faith in technology or reflexive resistance to innovation. It’s thoughtful integration that honors both human wisdom and algorithmic insights. Because when it comes to your health, you deserve better than one-size-fits-all solutions—you deserve precision medicine that treats you as the unique individual you are.
The future of nutrition isn’t about following rigid rules; it’s about algorithms that learn your story and adapt continuously to help you write the healthiest possible next chapter.
Recommended Reading:
“The definitive guide to intermittent fasting — a highly effective therapeutic approach that boosts well-being, supports weight loss, and delivers life-changing results.”
The Complete Guide to Fasting by Jason Fung
“Change your daily routine, transform your health.”
The Circadian Code by Satchin Panda
Sources:
- Zhong VW, et al. Association of eating in 8-hour time window with cardiovascular mortality. American Heart Association Scientific Sessions, 2024.
- Liu H, et al. Prediction of fasting status using supervised machine learning and wearable device data. Digital Health, 2023.
- Badran M, et al. Intermittent fasting after ST-elevation myocardial infarction: A pilot randomized controlled trial. Circulation, 2024;149(8):623-632.
- Potter GDM, et al. Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocr Rev, 2016;37(6):584-608.
Disclaimer: This educational content was developed with AI assistance by a physician. It is intended for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare professional for personalized guidance. The information provided is valid as of the date indicated at the end of the article.

Comments